Clinical trial led by Vanderbilt Health seeks to refine lung cancer biopsy standards
- Read more about Clinical trial led by Vanderbilt Health seeks to refine lung cancer biopsy standards
Vanderbilt Health investigators have received a grant from AstraZeneca to lead a multisite, randomized control trial aimed at refining the standard of care when using robotic bronchoscopy combined with three-dimensional imaging to obtain lung samples for malignancy assessment and gene sequencing.
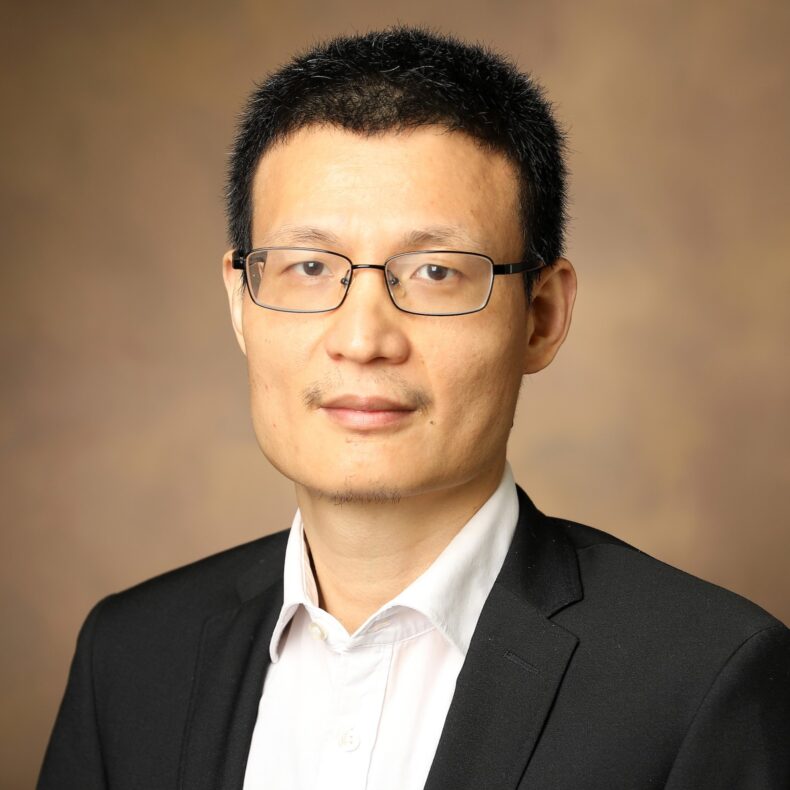
“Recent advances in minimally invasive bronchoscopic techniques have improved the diagnostic yield, particularly for peripheral pulmonary lesions, and in the recent VERITAS trial, we demonstrated that navigational bronchoscopy can achieve a diagnostic accuracy of around 79%,” said Fabien Maldonado, MD, MSc, professor of Medicine and Thoracic Surgery and director of Interventional Pulmonology at Vanderbilt Health. “That is statistically comparable to transthoracic needle biopsy, which is around 74% accurate.”

“Because of the proven success of navigational bronchoscopy, we now want to determine whether or not the rapid, on-site evaluation (ROSE) of biopsy material remains a necessary step. We’ll test the hypothesis that this advanced bronchoscopy procedure done without ROSE guidance is non-inferior to bronchoscopy with ROSE. This could have immediate patient care implications, potentially shortening procedure time, improving specimen quality and avoiding complications from additional, unnecessary biopsies.”
ROSE has been the standard of care for decades in navigational bronchoscopy, but it adds time, cost and may paradoxically result in lower quality specimens. It can also lead to complications from unnecessary biopsies motivated by unclear intraprocedural results. With modern techniques such as robotic bronchoscopy with cone-beam CT technology, which is rapidly becoming the standard of care, the need for ROSE needs to be studied, said Maldonado, Pierre Massion Director in Lung Cancer Research.
The development of better biopsy approaches is driven by the fact that lung cancer kills more than 130,000 Americans annually, and survival depends on early diagnosis, which requires biopsy to be definitive. Current approaches make accurate biopsy challenging or even impossible for many hard-to-reach lesions.
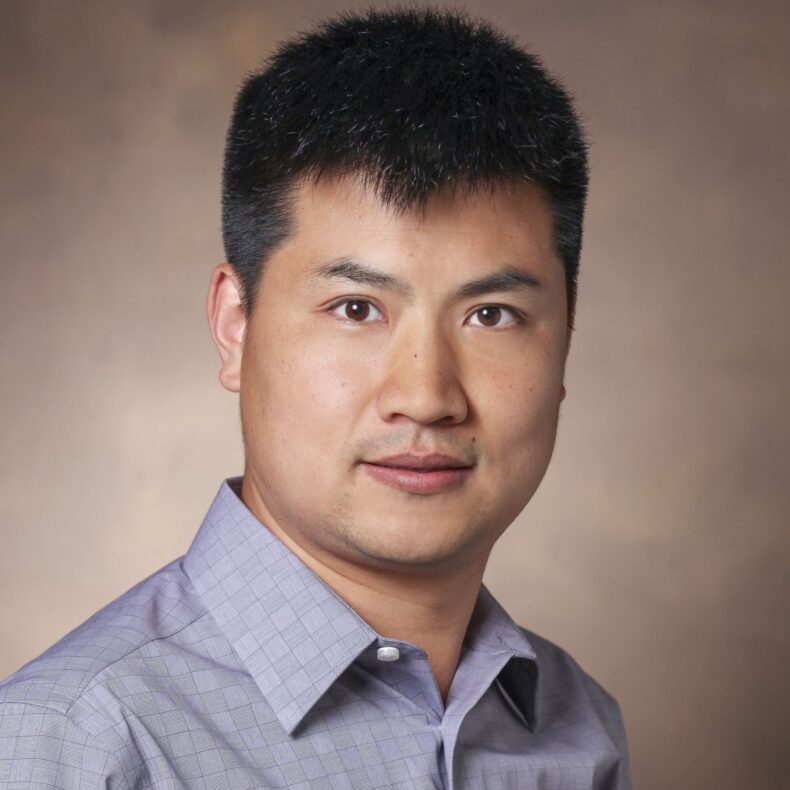
These modern bronchoscopy techniques extend the range of bronchoscopes and the ability to access lesions reliably and safely throughout the lung, including in the peripheral zone, said study co-investigator Rafael Paez, MD, MSCI, assistant professor of Medicine in the Division of Allergy, Pulmonary and Critical Care Medicine.
The Advanced Robotic Techniques and Rapid Onsite Evaluation for Minimally Invasive Diagnosis and Next-Generation Sequencing (ARTEMIS) trial will be conducted at Vanderbilt Health and nine other United States medical centers. Expected enrollment will be 440 adults who are scheduled for a navigational bronchoscopy for the evaluation of a pulmonary lesion. Participants will be randomized to have the procedure with the addition of ROSE or to have the procedure without ROSE.
The primary objective is to assess the diagnostic yield of robotic bronchoscopy with and without ROSE for peripheral lung lesions. A secondary objective is to compare the adequacy of malignant tissue samples for next-generational sequencing (NGS) between the two intervention strategies.
ROSE involves the immediate microscopic assessment of biopsy specimens, typically performed by a cytotechnologist or cytopathologist, to confirm the adequacy of biopsy samples obtained during a bronchoscopy for the diagnosis of malignancy. This has also been an important step in the past to ensure sufficient tissue is obtained for NGS to identify genetic mutations to guide treatment decisions, said Maldonado.
A 2023 Rapid On-site Evaluation Practice Variability Appraisal survey of interventional pulmonologists revealed significant variation in ROSE utilization. Of the 137 respondents, 88% reported ROSE availability, while time constraints (28%), availability of cytology (22%) and scheduling conflicts (20%) were the most reported barriers to ROSE utilization.
“Additional motivation for determining if ROSE use and non-ROSE use yield similar outcomes during diagnostic procedures is that ROSE is historically poorly reimbursed and uses considerable hospital resources,” Maldonado said. “Our findings will guide interventional pulmonologists in optimizing workflow and technology during robotic bronchoscopy, aiming to maintain the nearly 80% diagnostic yield seen in trials like VERITAS, thus improving patient care as we evaluate pulmonary lesions.”
The post Clinical trial led by Vanderbilt Health seeks to refine lung cancer biopsy standards appeared first on VUMC News.