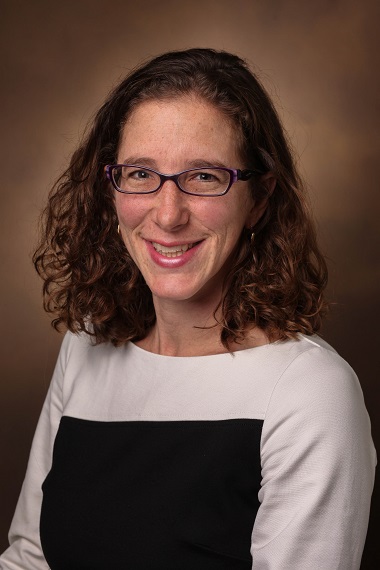
Marjan Rafat wins Biomedical Engineering Society Cellular and Molecular Bioengineering Young Innovator Award
Chemical and biomedical engineer and cancer researcher Marjan Rafat has received the Young Innovator Award from the Cellular and Molecular Bioengineering division of the Biomedical Engineering Society. The CMBE Young Innovator Award is a distinguished honor for young faculty in the biomolecular engineering field.